Neuropathic pain—burning, tingling, electric-shock-like pain—can make everyday life feel unbearable. When nerves are damaged, compressed, or sensitized, traditional painkillers often fall short.
At ALGOS Multispeciality Pain Clinic, we combine advanced technology with evidence-based treatments. One such technique making a difference in neuropathic pain management is Ultrasound-Guided Dry Needling.
Let’s explore how it works, where it helps, and why it’s a game-changer for chronic nerve pain.

What Is Neuropathic Pain?
Neuropathic pain occurs due to damage or dysfunction in the nerves. Unlike muscular or joint pain, this pain is more complex and can persist long after the initial injury.
Common causes include:
- Diabetic Neuropathy
- Post-Herpetic Neuralgia (Shingles Pain)
- Radiculopathy (sciatica, cervical/brachialgia)
- Post-surgical nerve pain
- Entrapment Neuropathies (Carpal tunnel, Meralgia Paresthetica, Tarsal Tunnel, etc.)
- Complex Regional Pain Syndrome (CRPS)
Symptoms often include:
- Burning or shooting pain
- Tingling, pins and needles
- Numbness or hypersensitivity
- Pain that worsens with light touch (allodynia)

What is Dry Needling?
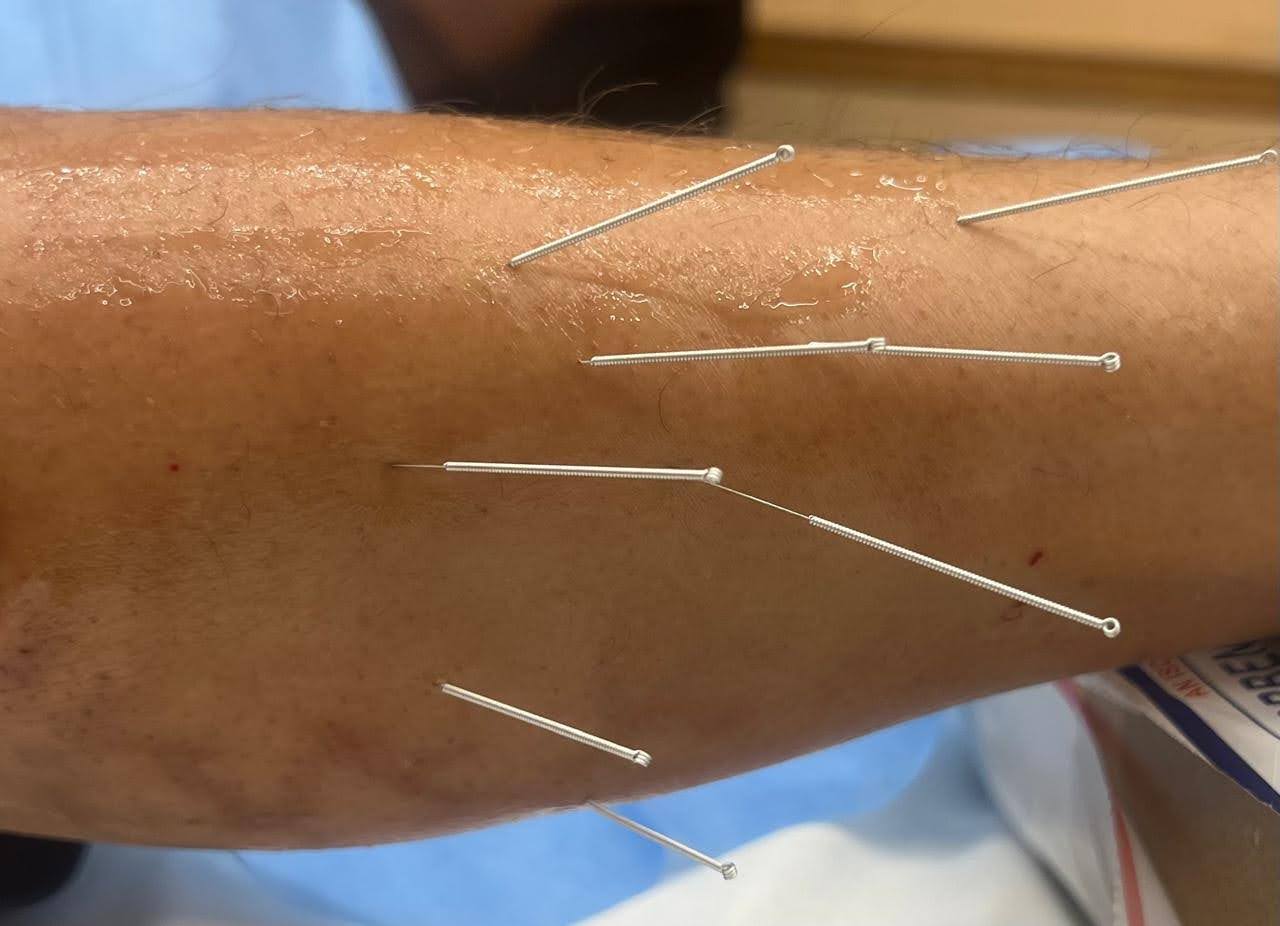
Dry needling involves inserting thin, sterile needles into trigger points, tight muscle bands, or near irritated nerves to:
- Reduce muscle spasm
- Release pressure on nerves
- Improve blood flow and oxygenation
- Modulate nerve sensitivity
It’s called “dry” because no medication is injected.

Why Use Ultrasound Guidance?
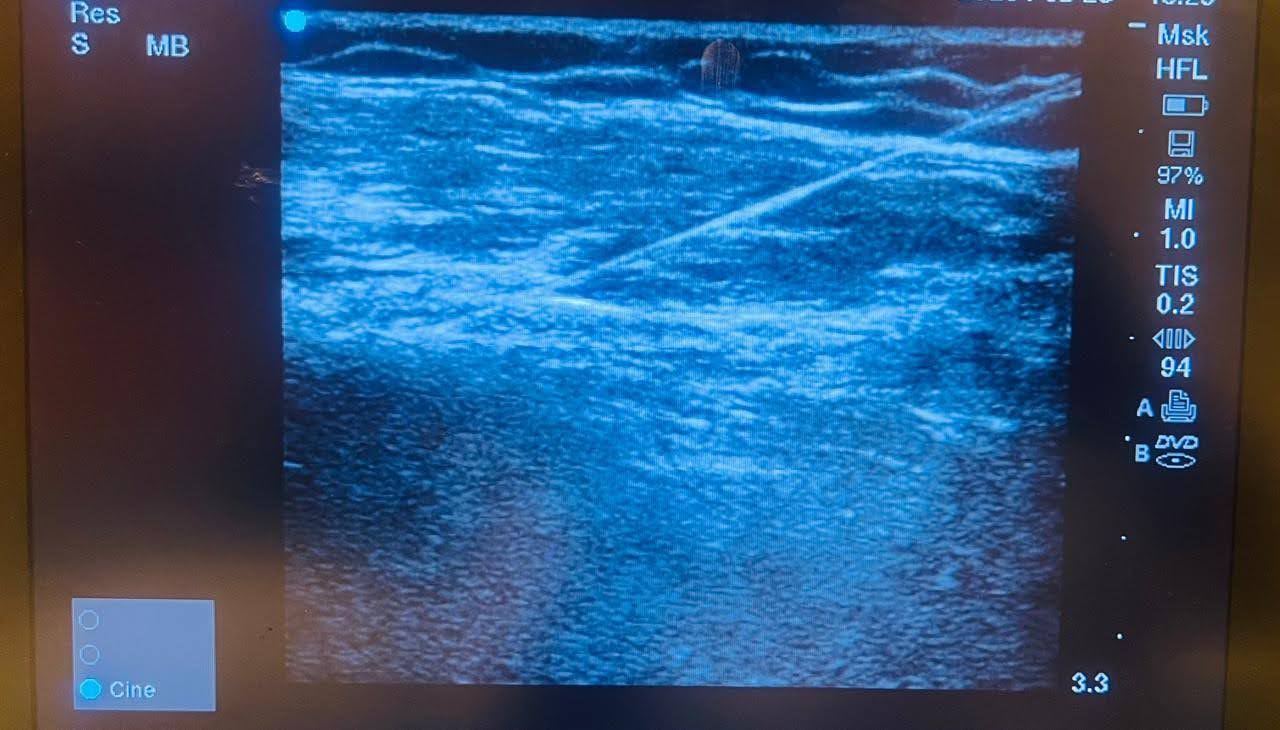
While traditional dry needling is based on surface anatomy and palpation, Ultrasound-Guided Dry Needling brings in:
- Precision – The needle is visualized in real-time, ensuring accurate placement near the nerve or muscle
- Safety – Avoids blood vessels, organs, and other critical structures
- Diagnostic Clarity – Helps identify fibrotic tissue, nerve entrapment, or fascial restrictions
This makes it especially useful for deeper structures and delicate areas, such as:
- Sciatic nerve
- Median or ulnar nerve
- Intercostal nerves
- Pudendal nerve
- Posterior tibial nerve
- Cervical paraspinals or thoracic outlet region

Conditions Where It Helps
At ALGOS Multispeciality Pain Clinic, we’ve successfully used ultrasound-guided dry needling in:
- Piriformis Syndrome & Sciatica
- Brachial Plexus Entrapment / Thoracic Outlet Syndrome
- Occipital Neuralgia
- Post-surgical scar neuropathy
- Diabetic small fiber neuropathy with myofascial component
- Trigeminal neuralgia (with facial trigger points)

What to Expect During the Procedure
- Initial evaluation and identification of the affected nerve or muscle
- Application of ultrasound gel and probe to visualize the area
- Thin needles are precisely inserted under real-time guidance
- You may feel a twitch or mild ache during needle insertion
- Minimal discomfort and quick recovery
Sessions typically last 20–30 minutes. Most patients feel relief after a few sessions, especially when combined with other therapies like nerve blocks, physiotherapy, or neuromodulation.

Advantages of Ultrasound-Guided Dry Needling
- Minimally invasive and drug-free
- Real-time precision targeting
- Reduced risk of complications
- Short recovery time
- Complements other treatments like nerve blocks or ozone therapy
At ALGOS Multispeciality Pain Clinic, our focus is on targeted, image-guided, and holistic pain relief. We use the latest technology—like ultrasound—to improve both diagnosis and treatment outcomes for neuropathic pain.
If you’re struggling with burning nerve pain or chronic tingling and sensitivity, dry needling could be the solution you’ve been waiting for.
To know more or book a consultation, call us at 7975896550 or write to info@algospainclinic.com.

REFERENCES
- Vas L. Effectiveness of ultrasound guided dry needling in chronic pain. Pain News. 2019;17:202–12.
- Travell JG, Simons DG. Myofascial Pain and Dysfunction: The Trigger Point Manual. Lippincott Williams & Wilkins. 1983
- Dommerholt J, Huijbregts P, editors. Myofascial Trigger Points: Pathophysiology and Evidence-Informed Diagnosis and Management. Jones & Bartlett Learning. 2010
- Jin F, Guo Y, Wang Z, Badughaish A, Pan X, Zhang L, et al. The pathophysiological nature of sarcomeres in trigger points in patients with myofascial pain syndrome: A preliminary study. Eur J Pain. 2020;24:1968–78. doi: 10.1002/ejp.1647.